What is neuroaffirming practice and how can it help young people in out-of-home care?
Apr 2024
Written by Jessica Wright Billy Black
The 2nd of April is World Autism Awareness Day, celebrating and promoting understanding and inclusiveness of people on the autism spectrum. In out-of-home care, neurodiversity is a highly prevalent and often overlooked contributor to how children and young people respond to care and care planning.
Therapeutic specialist Jessica Wright is a strong advocate for neuroaffirming practice, having seen many children in out-of-home care who struggle with trauma-based responses alongside neurodivergent traits. As children’s responses to trauma and neurodiversity are prone to overlap, many caring adults can struggle to easily identify and support the true roots of their children’s challenges.
I asked Jessica about neuroaffirming practice and what it means for the children she works with.
Happy World Autism Awareness Day! First of all, what is neuroaffirming practice?
Neuroaffirming practice is about understanding and accepting something called “neurodiversity”, so let’s start there.
While we’re all technically “neurologically diverse”, people with a typical neurobiology are described as “neurotypical”, while “neurodivergent” people may have any range of neurological difficulties. In this way, neurodivergence has become the umbrella term for autism, ADHD, dyspraxia, dyslexia, OCD, Tourette’s, bipolar, schizophrenia, and others.
So then “neuroaffirming practice” is neurodiversity-affirming practice, it’s accepting, affirming, including, and uplifting neurodivergence and actively considers how to work with each person in a way that suits them.
As a therapeutic specialist, how have you seen neurodiversity impacting children and young people in out-of-home care?
The really simple answer is that we are seeing the impacts every day. So many children we work with have flags for neurodivergence in their presentation or behaviour, but it isn’t attended to, because of other urgent priorities: finding a new placement, stabilising the current placement, parenting issues, all sorts of things. Often, their adults can only see these flags much later when their lives are more stable, but their dysregulation and presentation is still escalated.
But neurodiversity is highly prevalent in out-of-home care! Every child I work with either has flags raised for neurodivergence that we’re monitoring because they’re still in early childhood (<5 years old), or else they’ve been diagnosed but it’s difficult to get a diagnosis that clearly fits, because their presentation is so atypical due to the impact of trauma.
For instance, I work with a pre-teen, who had clear flags for autism from as early as 3 years old in their file. They weren’t diagnosed until 8 – it took five years and one really dedicated carer who understood their neurodevelopmental differences. And that also took luck; most kids don’t get fast-tracked for access to a funded programme with a psychologist, a speech pathologist, and a neuropsychologist who is able to assess. The carer strongly advocated for this programme, to her credit, but expecting carers to advocate places a significant burden on someone who’s already covering so many intense direct care needs.
Do you think neurodivergence in out-of-home care is getting the focus that it needs?
I think we’re seeing progress. I see younger neurodivergent kids I work with are attended to appropriately. Especially since the introduction of Early Childhood Early Intervention (ECEI) funding that does not require a diagnosis for children under 5. That funding helps adults understand behaviours and presentation earlier on, which can then lead to an earlier and better-informed diagnosis.
It’s a little easier to get support for little people, because we expect them to have big feelings and to be unkind sometimes. As they grow older and still use disconnection and rejection to protect themselves, children start getting labelled as “manipulative”, “controlling”, or “cruel”, which is so unhelpful.
For older children in out-of-home care, when they’ve missed out on early intervention and haven’t had a stable caring adult involved, neurodivergence is not the first thing on the allocated practitioner’s mind. The child protection system is under-resourced, and the presence of trauma-responsive behaviours can complicate what is inferred from children’s behaviour and presentation.
In the case of one child I work with, we’ve been able to ride out a period of extreme trauma-responsive behaviour through therapeutic parenting (– which will always help, regardless of neurodivergence! –) only to see the behaviours that still remain and consider that these were perhaps not responses to trauma but neurodivergence.
It’s harder to pick that out so easily for many older children in care. With a tumultuous placement history and many big behaviours, it’s harder to see a clear history of neurodivergent flags. Without a solid stable carer to see that, neurodivergence does get missed.
What do you think is an unseen challenge of providing the best care we can for neurodiverse children and young people in out-of-home care?
I think it’s really in seeing flags of neurodivergence in behaviour or presentation despite the impact of trauma, prioritising it as a consideration, obtaining a diagnosis, and incorporating neurodiversity-affirming care into trauma-informed care, amongst all the other care needs that children have.
The nuance of neurodiversity is not well understood, and the DSM5 doesn’t allow for a nuanced approach to diagnosing kids either. I work with two very socially motivated kids who are on the cusp, mere points away from a diagnosis of autism. But they are so socially motivated, because they’ve developed that to survive their childhoods, that they can easily mask those flags for an hour or two of observational assessment to please the assessor.
The trauma-responsiveness of this socially motivated behaviour makes sense as a survival strategy: “I need you to see me as good and loveable so I have to endear myself to you now, that way, you’ll tolerate how bad I am later”. These children may line up teddies and have echolalia and a long list of absolutely ASD traits, but that masking behaviour they use in assessment means they can’t get a diagnosis and can’t get access to support they really need.
What can we do differently in how we care for children and young people with trauma, if we’re aware that they may be neurodiverse?
Neuroaffirming practice and trauma-informed practice are really aligned! They are both about perceiving the child as good, valuable, worthy of love and good relationships just for who they are, accepting that we must make accommodations for their individual unique needs. For neurodivergent kids, that could be about attending to sensory needs in a different way, fitting the lights to be adjustable, having different options for music and smells and sounds, and a space that can be tailored for them.
Research tells us that neurodivergent children are far more likely to experience trauma, and of course, with a non-typical neurobiology you have a different communication system that can clash with a system not built for you, so you are more likely to be misunderstood and experience harm.
What trauma-informed carers and services could do is be more ready to accept that neurodivergence and trauma are often co-occurring. The two may be quite different root causes for children’s behaviour and presentation, but they are intrinsically connected and can be attended to as a whole single experience of the world, what feels safe, what feels threatening.
I’ve read in research as well, that living with sensory sensitives is itself like a constant mild trauma for children, which really aligns with what you’re saying about trauma and neurodivergence being so intrinsically linked.
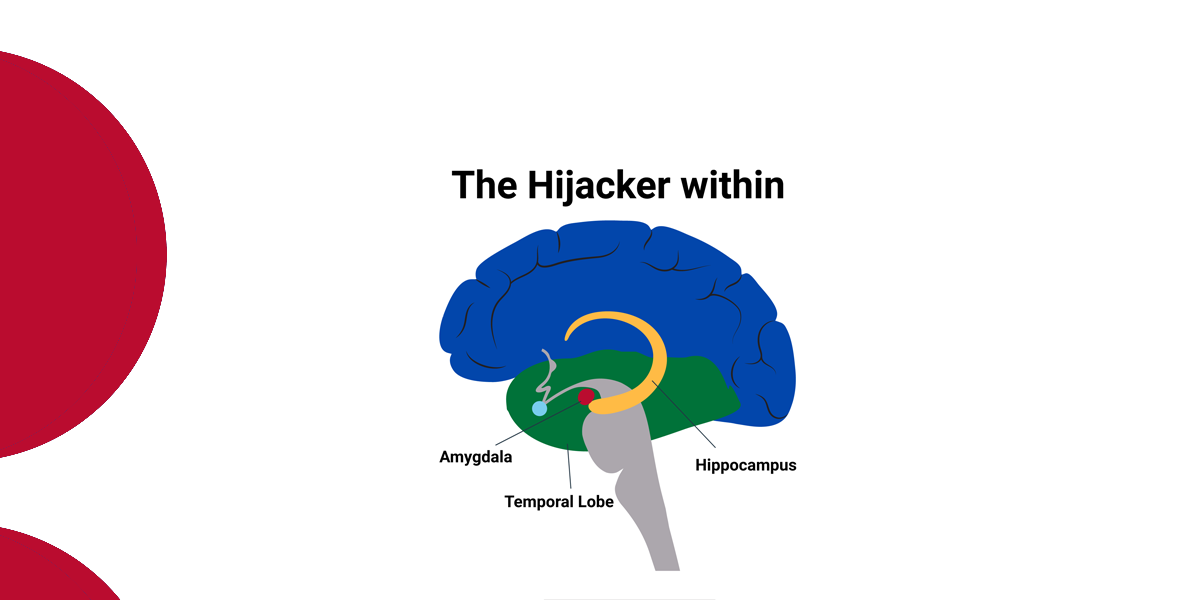
It is! Trauma really is just chronic stress. If the environment is too overwhelming and it isn’t tailored to meet your needs, that impacts your responses, which impacts your behaviours. Children become distressed and dysregulated, more likely to tip into hypo- or hyper-arousal.
One really big difficulty for some of our foster carers is things like being pushed away from a hug that might not be helpful for a child, which can feel like a very personal attack, that their love isn’t acceptable. Of course, it’s not their love, it’s the response itself that wasn’t helpful, but people can have a hard time separating out a response that feels rejecting. Then carers can start to withdraw from children, because our brains are such wonderful self-protectors, and can get into a cycle of blocked care: carers become less available, then behaviours escalate.
Neurodivergent nervous systems have more synapses due to having more connections than in a typical brain, which means more ability to receive more information – but that quickly becomes overwhelming. Without the right strategies in place to manage that, you’ll see the same behaviours as trauma-responsive behaviour, because it is a type of trauma response.
I think understanding these things about neurodivergence can feel scary because it’s a whole new thing to think about and learn in this space. But I think it quickly feels much more natural when you understand what it is, and what it’s not.
What I’m hearing is that a trauma-informed space, if it’s truly trauma-informed, is already an inclusive safe space for neurodiverse children because it adapts to individual children’s needs – so really, the big adaptation we could ask for is better awareness and understanding of neurodiversity from support workers?
Absolutely! Every child will have a different feeling of how neurodivergence is or isn’t part of their identity, what accommodations will work for them, and what support they find genuinely meaningful. It’s not enough to have gone to a training day and install a light switch dimmer, we need to continue attending to these needs over time. We adapt when sensory interests or special interests change, and we continue to check in with children as they grow different tolerances and get interests in different things.
Support workers have the power to help everyone supporting the child, and look at other supports too – it takes much more than a regular village to support a child in out-of-home care, let alone one with neurodivergence.
One incredible carer I work with cares for two siblings as well as three biological kids. There is so much more support needed than any one carer can provide. We have debriefs every couple of days, our fortnightly care teams, fortnightly visits to the child if they need it, school meetings. But just as important was that we fund the carer getting their own psychological support separate from our team, and a funded cleaner that comes fortnightly so she can keep up with caring for the children. If the carer is stressed, the children’s needs won’t be met. Caregivers need significant support to meet the needs of children with trauma, and especially neurodivergent children with trauma.
How do you see the future of trauma-informed approaches in out-of-home care evolving, as our awareness and understanding of neurodiversity increases over time?
My hope is that we keep seeing the two paradigms of trauma-informed care and neuroaffirming care sitting closer together, because neurodivergent children are more likely to experience trauma, be involved youth justice and the care system, and have a higher likelihood of comorbid conditions.
If you are being neurodiversity-affirming, that is a trauma-informed approach, because it sees the child or young person for who they are, separate from their stress behaviours. Either way, it’s an individualised approach to providing safe care, and the way you help people feel safe is by giving them safe relationships.
For a neurodivergent person, that relationship may look a little different, depending on how relationships feel safe to them, so it might not be initially comfortable for a clinician who’s used to doing relationships in a certain way. But ultimately, all children respond positively to feeling safe, so we can reduce their distress through relationship safety.